RRS(Rapid Response System)
RRSテキスト
Managing Deteriorating Patients 1st ed
We are indebted to our Japanese colleagues for translating the entire book so that it may reach a larger audience.
The project was supervised by:
Dr. Shigeki Fujitani
Dr. Kazuaki Atagi
Dr. Masatoshi Okumura
Specific chapters were translated by:
Dr. Masatoshi Okumura (Chapters 1,2,3)
Dr. Shinsuke Fujiwara (Chapters 4,5)
Dr. Hiromu Naraba (Chapters 6,7,8)
Dr. Kohei Yamada (Chapters 9,10)
Dr. Yoshihisa Fujimoto (Chapters 11,12)
Dr. Junichiro Iio (Chapters 13,14)
Dr. Shota Tanabe (Chapters 15,16)
Dr. Yasunobu Goto (Chapters 17,18)
RRSとは
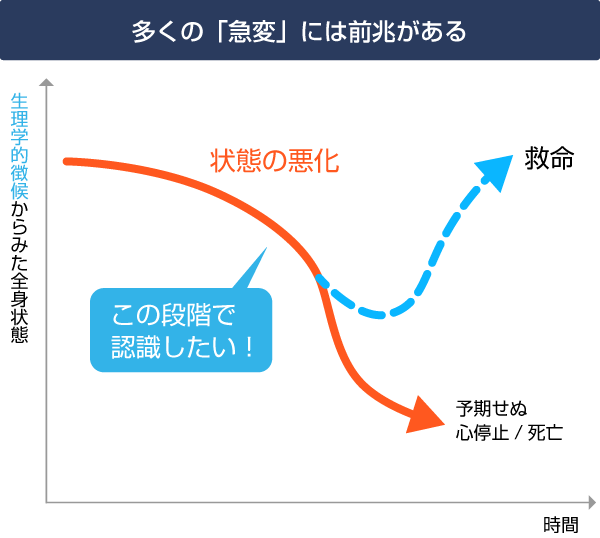 RRS=Rapid Response System(院内迅速対応システム)とは、多くの「急変」には前兆があるという点に着目した院内対応システムです。RRSでは早期認識と早期介入が重要です。
RRS=Rapid Response System(院内迅速対応システム)とは、多くの「急変」には前兆があるという点に着目した院内対応システムです。RRSでは早期認識と早期介入が重要です。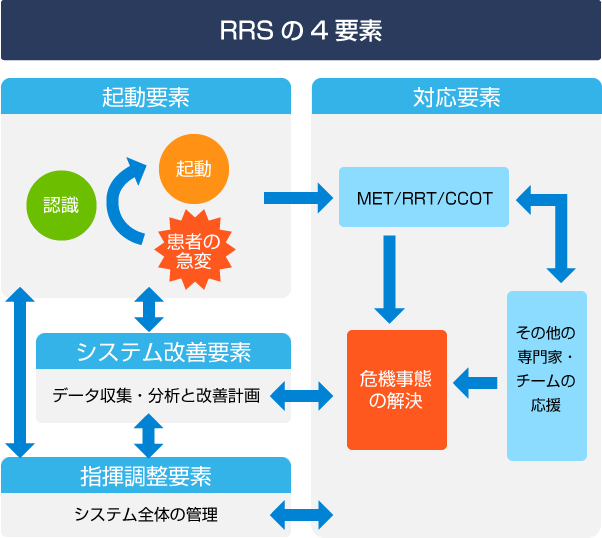 RRSは4つの要素から成ります。
RRSは4つの要素から成ります。
「RRS解説(IHECJ)」のファイル(パワーポイント)はこちらのリンクから無料でダウンロードできますので、各施設での啓発活動に役立ててください。
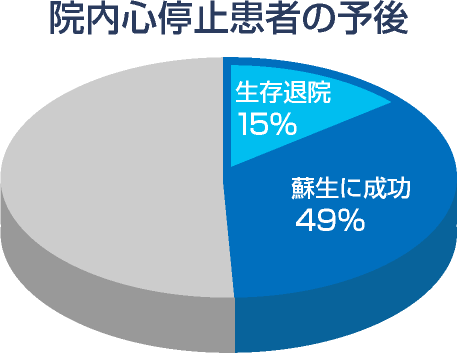
院内心停止(IHCA)とRRS
IHCA=In-Hospital Cardiac Arrest(院内心停止)
病院内だろうと、心停止に陥ってからの介入では予後が不良であることがわかっています。
前兆を捉え、システムで対応しましょう。
RRSの効果は院内心停止の減少で測られます。
用語集
RRSに関わる用語の日本語訳と定義が本委員会により2017年になされました。
システムに関する用語
- 用語
Rapid Response System (RRS) - 日本語訳
院内迅速対応システム - 定義
患者に対する重篤有害事象(別表を参照)を軽減することを目的とし、迅速な対応を要するバイタルサインの重大な増悪を含む急激な病態変化を覚知して対応するために策定された介入手段。以下の4つの要素から構成されたシステム全体を指す。
- 用語
Afferent limb / component - 日本語訳
起動要素(求心路) - 定義
病棟スタッフが患者の状態悪化を認識し、あらかじめ定められた起動基準に従って対応チームを起動すること。
- 用語
Efferent limb / component - 日本語訳
対応要素(遠心路) - 定義
病棟からの起動に応じて迅速に(15分以内が望ましい)現場に急行し、患者の評価と初期対応を行うこと。重篤な患者の安定化と管理に必要なスキルを備えたスタッフと、必要な資機材から成る。チーム構成によりMET、RRT、CCOTに大別される。
- 用語
Patient safety / process improvement limb / component - 日本語訳
システム改善要素 - 定義
発生した事案をデータ集積し、将来同様の事案を回避できるよう、管理・ケアの改善に役立つようフィードバックすること
- 用語
Governance / administrative structure limb / component - 日本語訳
指揮調整要素 - 定義
RRSを計画、導入し、維持運営する母体組織。スタッフへの教育や対応チーム構成の選任、資機材の整備などを司る。
対応チームに関する用語
- 用語
Medical Emergency Team - 日本語訳
MET - 定義
医師を1名以上含み、気管挿管などの二次救命処置をベッドサイドで開始できる能力を備えた対応チーム。
- 用語
Rapid Response Team - 日本語訳
RRT - 定義
医師を必ずしも含まず、起動された患者を評価し基本的な初期対応を行った上で、必要に応じて患者の院内トリアージや医師の緊急招請を行うチーム。
- 用語
Critical Care Outreach Team - 日本語訳
CCOT - 定義
集中ケアの訓練を受けた看護師らが主体となって、ICU退室患者と何らかの懸念のある入院患者を定期的に訪床して回り、起動基準に抵触する患者を早期発見することを目指した対応チーム。
アウトカムに関する用語
- 用語
Unexpected cardiac arrest - 日本語訳
予期せぬ心停止(事前DNARなし) - 定義
ICU外に入院中に、DNARが合意されていない、ないしは記載されていない患者で起こった心停止。
- 用語
Unexpected death - 日本語訳
予期せぬ死亡(事前DNARなし) - 定義
ICU外に入院中に、DNARが合意されていない、ないしは記載されていない患者で起こった死亡。
- 用語
Unexpected ICU admission - 日本語訳
ICU予定外入室 - 定義
ICU外に入院中の患者の、予定外でのICU入室。
- 用語
Serious adverse event (SAE) - 日本語訳
重篤有害事象 - 定義
予期せぬ心停止、予期せぬ死亡、およびICU予定外入室。
参考文献
- 文献
Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011;365(2):139-146.
http://www.ncbi.nlm.nih.gov/pubmed/21751906 - 説明
RRSを包括的に解説した最も有名な総説です。筆者はRRSの世界的な推進者の一人であり、多くの論文を執筆しています。
- 文献
Devita M a, Bellomo R, Hillman K, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006;34(9):2463-2478.
http://www.ncbi.nlm.nih.gov/pubmed/16878033 - 説明
RRSの用語や定義に関して初めて開催された国際会議の記録です。現在もここでの用語や定義が広く利用されています。
- 文献
Hillman K, Chen J, Cretikos M, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365(9477):2091-2097.
http://www.ncbi.nlm.nih.gov/pubmed/15964445 - 説明
RRSに関する唯一の無作為クラスラー割付による多施設比較研究です。23施設がRRS導入群と従来通りの急変対応群に割り付けられ、重篤有害事象の発生率が検討されました。残念ながら、この研究では両群間に有意差は見られませんでした。RRS導入群でも起動の遅い施設があった一方で、従来通りの急変対応群の中にも心停止に陥る前に”Code Blue”が起動される施設があったことが原因と後に分析されています。
- 文献
Cretikos M, Parr M, Hillman K, et al. Guidelines for the uniform reporting of data for Medical Emergency Teams. Resuscitation. 2006;68(1):11-25.
http://www.ncbi.nlm.nih.gov/pubmed/16153768 - 説明
RRSの4要素の一つである「システム改善要素」の核となるデータベースの構築に関して例示しています。
- 文献
Peberdy MA, Cretikos M, Abella BS, et al. Recommended guidelines for monitoring, reporting, and conducting research on medical emergency team, outreach, and rapid response systems: an Utstein-style scientific statement. A Scientific Statement from the International Liaison Committee on Resuscitat. Resuscitation. 2007;75(3):412-433.
http://www.ncbi.nlm.nih.gov/pubmed/17993369 - 説明
RRSの臨床研究を推進するために、院外心停止でも使用さているウツタイン方式の記録の利用を提唱しています。また、研究で見るべきアウトカムとしての有害事象についても検討されています。
- 文献
DeVita M a, Smith GB, Adam SK, et al. “Identifying the hospitalised patient in crisis”–a consensus conference on the afferent limb of rapid response systems. Resuscitation. 2010;81(4):375-382.
http://www.ncbi.nlm.nih.gov/pubmed/20149516 - 説明
RRSのシステムの成否を担う鍵とも言われる「起動要素」に関して開催された国際会議の記録です。バイタルサインからモニタリングまで、患者の観察について深い洞察が得られること請け合いです。
- 文献
Jones D, Lippert A, DeVita M, Hillman K. What’s new with rapid response systems? Intensive Care Med. 2014;41(2):315-317.
http://www.ncbi.nlm.nih.gov/pubmed/25427867 - 説明
上記のNEJMの総説の筆者が、RRSのより新しい知見を取り上げています。
- 文献
Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015;19:254.
http://www.ncbi.nlm.nih.gov/pubmed/26070457 - 説明
RRSが成人、小児を問わず、入院患者の病院死亡率や心停止発生率を減少させることを初めて証明したメタアナリシスです。
- 文献
Institute for Healthcare Improvement. 5 Million Lives Campaign.
http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Pages/default.aspx
Accessed on September 26th, 2016. - 説明
米国の医療安全管理団体による医療事故防止キャンペーン100,000 Lives Campaignの一環としてRRS導入が推進されてきました。現在はより包括的な取り組みとして5 Million Lives Campaignとして受け継がれています。
- 文献
The Joint Commission. National Patient Safety Goals.
https://www.jointcommission.org/standards_information/npsgs.aspx
Accessed on September 26th, 2016.
- 文献
National Institute for Health and Care Excellence. (NICE)
Acutely ill adults in hospital: recognising and responding to deterioration.
https://www.nice.org.uk/guidance/cg50
Accessed on September 26th, 2016. - 説明
英国の健康省によるガイドラインにもRRSの導入が収載されています。
- 文献
Australian Commission on Safety and Quality in Health Care. Recognising and Responding to Clinical Deterioration.
http://www.safetyandquality.gov.au/our-work/recognising-and-responding-to-clinical-deterioration/
Accessed on September 26th, 2016. - 説明
RRSの本家、豪州での医療安全管理団体によるウェッブサイト。
- 文献
医療安全全国共同行動.
http://kyodokodo.jp/10mokuhyou/1452-2/
Accessed on September 26th, 2016. - 説明
日本の多くの学会・団体が関与する医療安全管理キャンペーンです。「行動目標6:急変時の迅速対応」にRRSの確立が謳われています。
- 文献
Multicenter Comparison of Machine Learning Methods and Conventional Regression for Predicting Clinical Deterioration on the Wards.
Crit Care Med. 2016 Feb; 44(2): 368–374
http://www.ncbi.nlm.nih.gov/pubmed/26771782 - 説明
この多施設共同研究では、いくつかの機械学習法がロジスティック回帰よりも一般病棟での臨床悪化をより正確に予測する可能性がある。
- 文献
Real-Time Risk Prediction on the Wards: A Feasibility Study.
Crit Care Med. 2016 Aug;44(8):1468-73. doi: 10.1097/CCM.0000000000001716
http://www.ncbi.nlm.nih.gov/pubmed/27075140 - 説明
電子カルテベースの早期警告スコアである、電子心停止リスクトリアージスコアバージョン(eCART)を使用して、リアルタイムのリスク層別化の実現可能性と正確性を評価している。
- 文献
Deep Learning in the Medical Domain: Predicting Cardiac Arrest Using Deep Learning.
Acute and Critical Care 2018 August 33(3):117-120
https://www.accjournal.org/journal/view.php?number=1142
Accessed on May 22th, 2019. - 説明
Deep learning EWSは、高精度かつ低誤警報で心停止を予測する。DEWSは、あらゆる臨床環境で容易に取得できる4つのバイタルサインと精度を上げるための検査結果を用いる。
- 文献
Validating the Electronic Cardiac Arrest Risk Triage (eCART) Score for Risk Stratification of Surgical Inpatients in the Postoperative Setting: Retrospective Cohort Study.
Ann Surg. 2018 Jan 12. doi: 10.1097/SLA.0000000000002665.
Annals of Surgery. 269(6):1059–1063, JUN 2019
http://www.ncbi.nlm.nih.gov/pubmed/31082902 - 説明
早期警告スコアは術後患者の重篤な有害事象を予測するものであり、eCARTはこの患者集団においてNEWSおよびMEWSよりもはるかに正確です。
- 文献
An Algorithm Based on Deep Learning for Predicting In-Hospital Cardiac Arrest.
J Am Heart Assoc. 2018;7:e008678. DOI: 10.1161/JAHA.118.008678.
http://www.ncbi.nlm.nih.gov/pubmed/29945914 - 説明
多施設共同研究において、Deep learningに基づくアルゴリズムは、心停止患者の検出に対して高い感度と低い誤警報率を示した。
一般社団法人 日本蘇生協議会. JRC 蘇生ガイドライン. 東京: 医学書院; 2015
DNARオーダーとRRS
DNAR(do not attempt resuscitation)の定義は患者本人または患者の利益にかかわる代理者の意思決定をうけて心肺蘇生法をおこなわないことです。
ただし,患者ないし代理者へのinformed consentと社会的な患者の医療拒否権の保障が前提となります。欧米では実施のためのガイドラインも公表されています。
1995年日本救急医学会救命救急法検討委員会から「DNRとは尊厳死の概念に相通じるもので,癌の末期,老衰,救命の可能性がない患者などで,本人または家族の希望で心肺蘇生法(CPR)をおこなわないこと」,「これに基づいて医師が指示する場合をDNR指示(do not resuscitation order)という」との定義が示されています。
しかし,わが国の実情はいまだ患者の医療拒否権について明確な社会合意が形成されたとはいい難く,またDNR実施のガイドラインも公的な発表はなされていません。
なおAHA Guideline 2000では,DNRが蘇生する可能性が高いのに蘇生治療は施行しないとの印象を持たれ易いとの考えから,attemptを加え,蘇生に成功することがそう多くない中で蘇生のための処置を試みない用語としてDNAR(do not attempt resuscitation)が使用されています。
院内急変時に、DNARの確認を即座に行う工夫により、CPRを含むRRSの初動が円滑化されると考えています。(ある施設の取り組み)
参考文献
- 文献
The Medical Emergency Team System and not-for-resuscitation orders: results from the MERIT study
Resuscitation. 2008 Dec;79(3):391-7. doi: 10.1016/j.resuscitation.2008.07.021. Epub 2008 Oct 25.
http://www.ncbi.nlm.nih.gov/pubmed/18952354 - 説明
オーストラリアのコホート研究では、ほとんどの死亡は以前に文書化されNFR(not-for-resuscitation)オーダーの患者で発生したが、NFRオーダーは心停止コールまたは計画外のICU入院の前にはまれであった。METシステムを導入した病院では救急隊からより多くのNFR命令が出された。METの配分、病院の状態、病院の病床数、都市圏の所在地を考慮しても、NFRオーダーの差異の50%未満しか説明ができない。
- 文献
Enhanced end-of-life care associated with deploying a rapid response team: a pilot study.
J Hosp Med. 2009 Sep;4(7):449-52. doi: 10.1002/jhm.451
http://www.ncbi.nlm.nih.gov/pubmed/19753581 - 説明
当院にRRTを設置したことにより、根治治療を目的とした患者の転帰への影響はほとんどなく、RRTの導入は終末期の疼痛管理および心理社会的ケアの全般的改善と関連していた。
- 文献
Rapid response team calls to patients with a pre-existing not for resuscitation order
The rapid response system and end-of-life care.
Curr Opin Crit Care. 2013 Dec;19(6):616-23. doi: 10.1097/MCC.0b013e3283636be2.
http://www.ncbi.nlm.nih.gov/pubmed/19753581 - 説明
NFR(not-for-resuscitation)の事前指示のある患者へのRRTの要請はまれではない。最も一般的なのは何らかの懸念であり、起動時に呼吸関連の異常が観察され、同様の介入レベルが必要であり、ICUへの入室はより少なく、2回目以降の RRT起動時には、NFR(not-for-resuscitation)の指示がでている。
RRTの3分の1までが、終末期に関係している。これらの患者をよく理解することで、より入院患者のACPを改善に導く。
- 文献
The rapid response system and end-of-life care.
Curr Opin Crit Care. 2013 Dec;19(6):616-23. doi: 10.1097/MCC.0b013e3283636be2.
http://www.ncbi.nlm.nih.gov/pubmed/23799463 - 説明
RRTの3分の1までが、終末期に関係している。これらの患者をよく理解することで、より入院患者のACPを改善に導く。
- 文献
The medical emergency team call: a sentinel event that triggers goals of care discussion
Crit Care Med. 2014 Feb;42(2):322-7. doi: 10.1097/CCM.0b013e3182a27413.
http://www.ncbi.nlm.nih.gov/pubmed/23989179 - 説明
RRSの導入は、DNRの増加と関連していた。前哨イベントとして、METの起動とCCUへの移動は、治療のゴール検討をより促進し、しばしば 緩和ケア戦略へつながる。
- 文献
Rapid response systems: are they really effective?
Crit Care. 2015 Mar 16;19:104. doi: 10.1186/s13054-015-0807-y.
http://www.ncbi.nlm.nih.gov/pubmed/25887250 - 説明
他の研究では、MET介入によるDNARオーダーの指示の割合はさらに高く、最大24.6%である。
- 文献
Pre-existing risk factors for in-hospital death among older patients could be used to initiate end-of-life discussions rather than Rapid Response System calls: A case-control study.
Resuscitation. 2016 Dec;109:76-80. doi: 10.1016/j.resuscitation.2016.09.031. Epub 2016 Oct 18.
http://www.ncbi.nlm.nih.gov/pubmed/27769903 - 説明
RRSへの関与を必要とする高齢の悪化した患者のサンプルでは、慢性疾患、認知障害および虚弱性の複数の指標が死亡リスクの高さと実質的に関連していた。限定的な治療をするよりも無益な介入を防ぐ可能性がある終末期医療の議論を開始することを臨床医に知らしめていく必要がある。
- 文献
Who Benefits from Aggressive Rapid Response System Treatments Near the End of Life? A Retrospective Cohort Study.
Jt Comm J Qual Patient Saf. 2018 Sep;44(9):505-513. doi: 10.1016/j.jcjq.2018.04.001. Epub 2018 Jun 27.
http://www.ncbi.nlm.nih.gov/pubmed/30166034 - 説明
臨床転帰不良および死亡に明らかに関連する同定可能な危険因子は、より消極的な治療を施すための指針として使用することができる。
そのようなより消極的な対応策には、ICU移動への再検討、NFRオーダーへの順守、およびRRSチーム起動よりも、終末期医療への移行がある。